The Male Reproductive System — a clear, science-first guide (but chill)
An accurate walk-through of how the male reproductive system is built and how it actually works — peeing, erections, where sperm and semen come from, how everything coordinates, and what can mess it up. Science-forward, plain-English, and a little goofy because anatomy is wild. Let’s go.
—
Quick TL;DR
Peeing = bladder contracts, sphincters relax.
Ejaculation = coordinated sympathetic + somatic response; bladder neck closes so semen leaves the body, not the bladder.
Testes are ~2–4 °C cooler than body (~33–35 °C) because sperm like it chilly.
Erection = NO → cGMP → smooth muscle relaxation → blood fills corpora cavernosa; tunica albuginea traps the blood.
Sperm are made in the seminiferous tubules (~64–74 days), then finish maturing in the epididymis. Semen = sperm + fluids from seminal vesicles, prostate, and bulbourethral glands.
Many medical, lifestyle, or environmental things can reduce function or fertility — heat, varicocele, infections, steroids, obesity, smoking, etc.
—
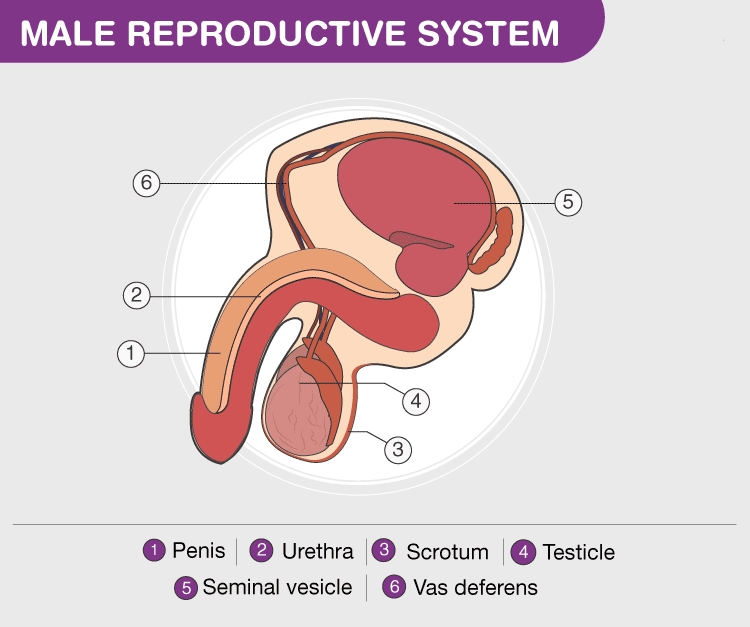
1 — Quick anatomy map (the basics)
Testes (testicles) — two egg-shaped organs in the scrotum. Make sperm and testosterone.
Epididymis — a long coiled tube on the back of each testis where sperm mature and are stored.
Vas deferens (ductus deferens) — the tube that carries sperm from epididymis toward the urethra during emission.
Seminal vesicles — behind the bladder; add most of the fluid (fructose, prostaglandins, etc.).
Prostate gland — under the bladder; adds enzymes, citrate, zinc, and factors that help semen liquefy and sperm move.
Bulbourethral (Cowper’s) glands — tiny; make pre-ejaculate to lubricate and neutralize urethral acidity.
Urethra — the tube inside the penis that carries urine and (during ejaculation) semen out. Segments: prostatic, membranous, penile (spongy).
Penis — shaft + glans; erectile tissues: two corpora cavernosa and one corpus spongiosum (around urethra).
Scrotum — pouch holding testes; muscles adjust position and temperature.
—
2 — How does male pee? (short and clean)
Short: kidneys → bladder storage → brain + spinal cord decide → bladder contracts and sphincter(s) relax → urine out the urethra.
Longer: urine is made in the kidneys, stored in the bladder. When the bladder stretches, mechanoreceptors send signals to the sacral spinal cord and brain. When you choose to pee:
1. Brain sends parasympathetic signals → detrusor (bladder) contracts.
2. Internal urethral sphincter (smooth muscle at bladder neck) relaxes.
3. External urethral sphincter (voluntary skeletal muscle) relaxes.
4. Urine flows through the urethra and out.
Important coordination: during ejaculation the internal sphincter closes so semen can’t flow backward into the bladder (prevents retrograde ejaculation). So the body has a “pee mode” and an “ejaculate mode” — they’re mutually exclusive most of the time.
—
3 — Average body temperature and scrotal/testicular temperature
Core (body) temp: roughly 36.1–37.2 °C (97–99 °F).
Scrotal/testicular temp: usually ~2–4 °C cooler than core — about 33–35 °C (91–95 °F).
Why colder? Spermatogenesis prefers a few degrees below core temp. The body uses:
Pampiniform plexus (venous network) for countercurrent cooling of arterial blood.
Cremaster muscle adjusts distance to body.
Dartos muscle changes scrotal skin tightness.
Practical tip: frequent hot baths, tight underwear, laptops on laps, or fever can raise scrotal temp and transiently lower sperm quality.
—
4 — How does the penis get hard? (erection physiology — plain)
Erection is mainly a vascular event controlled by the nervous system:
1. Arousal (sensory, visual, mental or physical) triggers parasympathetic nerves (S2–S4).
2. Nerves release nitric oxide (NO) in penile tissue.
3. NO increases cGMP in smooth muscle → smooth muscle relaxation.
4. Cavernous arteries dilate → blood fills sinusoids in the corpora cavernosa.
5. Tunica albuginea compresses venous outflow so blood gets trapped → rigidity.
6. Sympathetic activity later causes detumescence (flaccidity) and mediates emission/ejaculation.
Medical aside: PDE5 inhibitors (sildenafil/Viagra) block the enzyme that breaks down cGMP, so cGMP lasts longer and erections are easier to achieve.
—
5 — Where sperm and semen come from (spermatogenesis + accessory glands)
Spermatogenesis (where sperm are made)
Location: seminiferous tubules inside testes.
Cells involved:
Sertoli cells — nurse cells; form the blood–testis barrier and support developing sperm.
Leydig cells — in interstitial tissue; produce testosterone (stimulated by LH).
Big picture stages:
1. Spermatogonia (stem cells) divide → some stay stem cells, some become primary spermatocytes.
2. Meiosis I & II → ultimately produce four haploid spermatids.
3. Spermiogenesis → spermatids remodel (tail, condensed nucleus, acrosome) into spermatozoa.
Timing: full journey from stem cell → mature sperm ≈ 64–74 days, plus a couple weeks in the epididymis to gain motility/maturity.
Hormonal control (HPG axis)
Hypothalamus: pulsatile GnRH.
Pituitary: LH and FSH.
LH → Leydig cells → testosterone.
FSH → Sertoli cells → supports spermatogenesis.
Feedback: testosterone and inhibin B (from Sertoli cells) suppress GnRH/LH/FSH.
Semen (what’s actually ejaculated)
Sperm — small volume but crucial.
Seminal vesicles (~50–70% of ejaculate volume): fructose (energy), prostaglandins, fibrinogen-like proteins.
Prostate: citrate, enzymes (PSA), zinc; helps liquefy semen after ejaculation.
Bulbourethral glands: pre-ejaculate for lubrication and neutralization.
Typical volume: ~1.5–5 mL per ejaculation (varies widely).
Reference sperm concentration: WHO reference around ≥15 million/mL is considered within the typical reference range — but fertility depends on count, motility, morphology, volume, pH, etc.
—
6 — How erection, emission, ejaculation, and urination coordinate
Erection: parasympathetic-driven (point).
Emission: sympathetic-driven (shoot) — vas deferens, seminal vesicles, prostate contract to dump contents into the prostatic urethra. Internal sphincter closes.
Expulsion (ejaculation): somatic (pudendal nerve) triggers rhythmic contractions of pelvic floor muscles (bulbospongiosus) to expel semen.
Urination: only resumes after the sphincter resets and the parasympathetic/somatic balance switches back.
These are tightly timed so pee and ejaculate don’t mix — unless there’s surgical damage, certain meds, or rare conditions causing retrograde ejaculation.
—
7 — A quick timeline of orgasm/ejaculation
1. Arousal → erection.
2. Plateau → glands prep secretions; heart rate/blood pressure up.
3. Emission → sperm + glandular fluids move into urethra (sympathetic).
4. Expulsion/Ejaculation → pelvic muscle contractions eject semen; orgasm usually occurs here.
5. Resolution → detumescence; refractory period (time before another erection) — varies a lot between people and by age.
—
8 — Things that affect function & fertility
Heat exposure — hot tubs, tight clothing, laptops.
Varicocele — dilated scrotal veins that raise local temperature and oxidative stress.
Infections — mumps orchitis, STIs (e.g., chlamydia) can damage testes/ducts.
Hormonal disorders — low T, pituitary problems.
Medications & drugs — anabolic steroids, chemo, some psychiatric meds.
Lifestyle — smoking, heavy alcohol, poor diet, obesity, stress.
Age — sperm quality declines gradually with age.
Obstruction — block in vas deferens or epididymis → azoospermia (no sperm in ejaculate).
If worried: common first steps are a semen analysis, hormone tests, scrotal ultrasound (e.g., to check for varicocele), and review of medical/medication history.
—
9 — Common quick Q&A people ask
Can you pee and ejaculate at the same time? Usually no — internal sphincter prevents it. Retrograde ejaculation can occur with certain surgeries or meds.
Does circumcision affect sexual function? Generally no major effect on erectile function or fertility; sensitivity perception may change for some.
How long to make new sperm? About 2–3 months (~64–74 days) plus epididymal maturation.
Does tight underwear lower fertility? Possibly — tight underwear can raise scrotal temp. The evidence is mixed, but switching to looser underwear is an easy precaution if fertility is a concern.
When to see a doctor? Persistent pain, lumps in testis, sudden changes in erection/ejaculation, difficulty urinating, or fertility concerns.
—
10 — Anatomy & microanatomy (deeper detail)
Seminiferous tubules: site of spermatogenesis; lined with Sertoli + germ cells.
Leydig cells: in interstitium; testosterone producers.
Blood–testis barrier: Sertoli cell tight junctions protect developing sperm from immune attack.
Erectile tissue: corpora cavernosa = cavernous sinusoids lined by endothelium; tunica albuginea surrounds them. Corpus spongiosum surrounds urethra and prevents collapse during erection.
Nerves: dorsal nerve of the penis (somatic sensory), cavernous nerves (parasympathetic autonomic), sympathetic fibers for emission/detumescence.
Lymph drainage: testes → para-aortic nodes; scrotum → superficial inguinal nodes.
—
11 — Hormonal control (a bit more nuance)
GnRH pulse frequency affects LH vs FSH output.
Testosterone supports spermatogenesis (intracrine/paracrine action at high local levels), libido, muscle mass, bone density, erythropoiesis.
Inhibin B from Sertoli cells selectively suppresses FSH.
Stress, obesity, chronic illness, and certain drugs can disrupt the HPG axis and lower testosterone/sperm output.
—
12 — Semen chemistry & advanced notes
Liquefaction: semen is gel-like just after ejaculation; prostatic enzymes liquefy it so sperm can swim.
Capacitation: latent maturational process in the female tract that allows sperm to fertilize the egg.
pH: seminal fluid helps neutralize vaginal acidity to protect sperm.
Sperm quality metrics: count, motility (progressive vs non-progressive), morphology, volume, pH, liquefaction time, viscosity.
Genetic/epigenetic factors: sperm DNA fragmentation and epigenetic changes from lifestyle/toxins can affect fertility and offspring health.
—
13 — Common conditions (short list)
Infertility causes: varicocele, obstruction, hormonal issues, genetic conditions (e.g., Klinefelter’s), infections.
Erectile dysfunction (ED): vascular, neurologic, hormonal, or psychological causes. Vascular disease and diabetes are big players.
Peyronie’s disease: fibrous plaques in tunica albuginea → curvature.
Testicular cancer: often a painless lump; most common in ages ~20–35.
Prostate issues: BPH, prostatitis, prostate cancer.
STIs: can compromise fertility if untreated.
—
14 — Lifestyle & practical tips
Avoid long, frequent hot baths if trying to optimize sperm.
Use looser underwear if fertility matters.
Don’t place laptops directly on your lap for long sessions.
Maintain healthy weight, avoid smoking/excess alcohol, manage stress.
Check meds with a doc if you’re trying to conceive — some prescriptions and supplements (e.g., anabolic steroids) can suppress sperm production.
—
15 — Advanced science extras (short)
Spermatogenesis timing: ~64–74 days, then 2–3 weeks in epididymis.
Sperm motility types: progressive (good), non-progressive, immotile.
Acrosome reaction: enzymes released by sperm to penetrate the egg.
DNA fragmentation & epigenetics: matters for fertility and embryo health; lifestyle can influence epigenetic marks.
—
Final summary (TL;DR again, because retention)
The male reproductive system is a coordinated set of glands, ducts, muscles, nerves, and blood vessels.
Peeing and ejaculation are separate coordinated programs — bladder neck closes during ejaculation.
Sperm are built slowly in the testes (~2–3 months) and need cooler temps to be healthy.
Erections are vascular events triggered by parasympathetic nerves and NO/cGMP signaling; ejaculation is a sympathetic + somatic orchestration.
Fertility & sexual function depend on hormones, blood flow, nerves, temperature, and overall health — lots of modifiable things can help or harm.