An accurate walk-through of how the female reproductive system is built and how it actually works — periods, ovulation, where eggs and hormones come from, how conception happens (or doesn’t), and what can mess it up. Science-forward, plain-English, and mildly stunned that biology actually pulled this off.
Quick TL;DR
Period = shedding of the uterine lining when pregnancy doesn’t happen.
Ovulation = an egg released from the ovary ~once/cycle, usually ~14 days before the next period.
Fertilization usually happens in the fallopian tube (ampulla); embryo implants in the uterus ~6–10 days later.
Hormones (HPG axis): GnRH → FSH/LH → ovaries → estrogen & progesterone; feedback loops from estrogen, progesterone, and inhibin.
Fertility window ≈ 6 days (sperm can survive ~up to 5 days; egg viable ~12–24 hours).
Ovarian reserve is finite — eggs formed before birth and decline with age (big drop after ~35).
Sexual arousal involves clitoral erection, vaginal lubrication, pelvic floor contractions; orgasm involves somatic and autonomic reflexes.
Lots can affect function: PCOS, endometriosis, infections, smoking, obesity, chemo, age, etc.
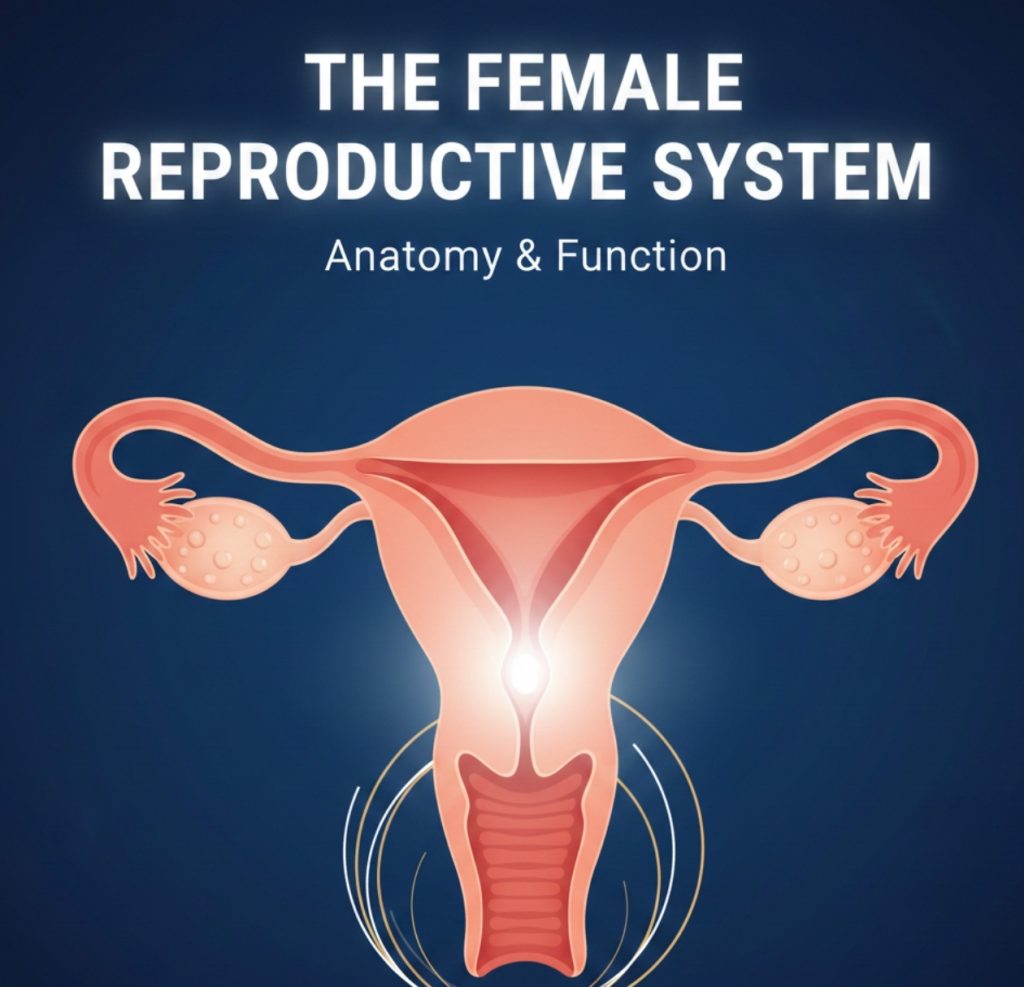
1 — Quick anatomy map (the basics)
Ovaries — two almond-shaped organs that make eggs (oocytes) and sex hormones (estrogen & progesterone).
Fallopian tubes (uterine tubes) — tubes that capture the ovulated egg and are the usual site of fertilization (ampulla region).
Uterus (womb) — muscular organ where the embryo implants and the fetus develops; lining = endometrium.
Cervix — lower narrow part of the uterus opening into the vagina; makes mucus that changes across the cycle.
Vagina — elastic canal; receives penis, serves as birth canal, and allows menstrual flow out.
Vulva — external genitalia (labia majora/minora, clitoris, vestibule, urethral opening).
Clitoris — highly innervated erectile organ; main sensory engine for sexual pleasure.
Bartholin’s glands (vestibular) — small glands near vaginal opening that add lubrication during arousal.
Pelvic floor muscles — support pelvic organs and contribute to orgasmic contractions.
Urethra — separate tube for urine; in females it’s short and opens into the vulval vestibule.
2 — How does peeing work (short & clean) — female edition
Same basic idea as males but with different anatomy: kidneys → bladder → urethra. The urethra is short in females, which is why UTIs are more common. Pelvic floor and sphincter muscles control continence. Sexual and urinary systems are physically close but separate functional systems.
3 — Egg-making: oogenesis & ovarian basics
Eggs are mostly ancient: all the oocytes a person will ever have form in the fetal ovary. They’re arrested in prophase I as primary oocytes until recruited later.
Each cycle some follicles begin to grow; one (usually) becomes the dominant follicle and completes meiosis I just before ovulation to become a secondary oocyte arrested in metaphase II. Meiosis II only completes if fertilization occurs.
Follicles contain the oocyte + supporting granulosa and theca cells that produce estrogen.
Timeline: unlike sperm, eggs are not continuously made — the supply declines with age through atresia. Fertility gradually declines, with a more pronounced drop after age ~35 and steep after ~40. Menopause is the end of ovarian function (average ~51 years).
4 — The menstrual cycle — hormones, phases, and what actually happens
Cycle length varies (commonly ~24–38 days). Key phases (simple version):
Follicular phase (period → ovulation)
Follicle recruitment → rising estrogen from granulosa cells.
Estrogen rebuilds the endometrium (the uterine lining) after menstruation and changes cervical mucus to be thin and sperm-friendly near ovulation.
FSH stimulates follicle growth; LH surge triggers ovulation.
Ovulation
LH surge → dominant follicle releases the secondary oocyte (egg). Usually ~14 days before the next period, not always day 14 of the cycle. Timing is relative to the next bleed, not the previous one.
Luteal phase (ovulation → next period)
The ruptured follicle becomes the corpus luteum, secreting progesterone (and some estrogen).
Progesterone stabilizes and gears the endometrium for implantation.
If no pregnancy → corpus luteum degenerates → progesterone falls → endometrium sheds (menstruation).
Key hormones: GnRH (hypothalamus) → FSH & LH (pituitary) → estrogen & progesterone (ovaries). Feedback loops regulate the rhythm; inhibin helps suppress FSH.
5 — Fertilization, implantation, and early pregnancy (short practical timeline)
Fertilization window: sperm can survive in the female tract up to ~5 days; the egg is viable ~12–24 hours after ovulation. So fertile window ≈ 5 days before → day of ovulation.
Where fertilization happens: usually the ampulla of the fallopian tube.
Zygote → blastocyst: fertilized egg divides while moving to the uterus. By ~5–6 days it becomes a blastocyst.
Implantation: blastocyst attaches to endometrium ~6–10 days post-ovulation (this is when hCG starts to rise after implantation).
Early pregnancy hormone: hCG from the implanting embryo maintains the corpus luteum until the placenta takes over progesterone production.
6 — Sexual arousal & orgasm — the female mechanics (plain)
Arousal: parasympathetic nerves (S2–S4) drive clitoral erection (engorgement) and vaginal lubrication (vaginal transudation + Bartholin’s glands + cervical mucus changes). Increased blood flow swells labia and clitoris.
Physiology: NO-mediated vasodilation contributes to clitoral/vestibular engorgement (similar molecular players to penile erection).
Orgasm: somatic (pudendal) and autonomic reflexes produce rhythmic pelvic floor (bulbocavernosus, pubococcygeus) contractions and a subjective peak of pleasure. Not everyone has the same pattern or needs penetration to orgasm — the clitoris is often the biggest player.
Resolution & refractory: many — but not all — people have a short resolution phase and can have multiple orgasms; refractory periods are usually shorter than in typical male physiology.
7 — Coordination: sex, contraception, and urine
Because the urethra is separate, urination and sexual function typically don’t conflict.
Contraceptives: hormonal (pill/patch/ring/injection/IUD that releases progestin) work mainly by preventing ovulation, thickening cervical mucus, and changing endometrium; IUDs (copper or hormonal) can prevent fertilization or implantation depending on type. Barrier methods (condoms, diaphragms) block sperm physically. Emergency contraception can reduce pregnancy risk after unprotected sex (timing matters).
Note on pregnancy prevention: methods differ in mechanism, reliability, and side effects — check a clinician for personalized advice.
8 — Timeline of conception/menstrual events (quick chronology)
Follicle growth (days vary) → rising estrogen.
LH surge → ovulation (egg released).
Fertilization possible in tubes (egg viable ~12–24 hrs; sperm up to ~5 days).
Blastocyst forms and implants ~6–10 days post-ovulation.
Implantation → hCG rises; missed period often first sign.
Pregnancy measured as ~40 weeks from last menstrual period (LMP).
9 — Things that affect function & fertility
Age — biggest single factor; quantity and quality of oocytes decline with age.
PCOS (polycystic ovary syndrome) — common hormonal disorder causing irregular cycles and anovulation.
Endometriosis — endometrial tissue outside the uterus causing pain and sometimes fertility trouble.
Tubal disease — scarring/obstruction (from infections like PID or surgery) can block egg-sperm meeting and cause ectopic pregnancy.
Uterine factors — fibroids, congenital anomalies, polyps can affect implantation or pregnancy.
Lifestyle & environment — smoking, obesity, heavy alcohol, certain toxins, and chemo can harm fertility.
Medications & medical conditions — some medicines, chemo, radiation, autoimmune disease can disrupt ovarian function.
Thyroid & prolactin disorders can mess with cycles.
Infections — PID from STIs can damage tubes/ovaries.
If worried: common first steps are cycle tracking, pelvic exam, ultrasound, hormone testing (FSH, LH, estradiol, AMH), and, if trying to conceive, semen analysis for the partner and fertility workup.
10 — Common quick Q&A people ask
Can you ovulate more than once a cycle? Usually one dominant ovulation per cycle, but rare cases (e.g., superfetation is basically nonexistent in humans). Sometimes closely spaced double ovulation can produce fraternal twins.
When’s the best time to try for a baby? The 5 days before ovulation + day of ovulation (fertile window).
Does breastfeeding prevent pregnancy? Lactational amenorrhea can suppress ovulation but is not 100% reliable unless strict conditions are met.
How long to try before seeing a doc? Common guideline: try for 12 months if under 35, or 6 months if 35 or older — then seek fertility evaluation.
Does period length mean anything? Variation is normal; very irregular cycles, very heavy bleeding, or severe pain merit medical attention.
11 — Anatomy & microanatomy (deeper detail)
Ovary histology: follicles at different stages (primordial → primary → secondary → Graafian) with granulosa & theca layers; corpus luteum after ovulation.
Endometrium: functional layer (sheds) vs basal layer (regenerates). Progesterone makes the lining secretory and receptive to implantation.
Fallopian tube microanatomy: ciliated epithelium helps transport the egg/embryo; secretions support early embryo.
Clitoral structure: glans, body, and two crura (erectile tissues) — not just a tiny external nub; much of it is internal.
Innervation: pelvic splanchnic nerves (parasympathetic) for arousal; hypogastric/sympathetic for other functions; pudendal nerve for somatic sensation and pelvic floor control.
Lymph drainage: ovaries → para-aortic nodes; uterus → internal iliac nodes; vulva → superficial inguinal nodes.
12 — Hormonal control (nuance)
GnRH pulse frequency matters — changes how much LH vs FSH is released.
Estrogen (estradiol) has proliferative effects on the endometrium and drives many secondary sexual characteristics and libido.
Progesterone prepares the endometrium for implantation and suppresses further ovulations in the luteal phase.
Inhibin from granulosa cells suppresses FSH.
AMH (anti-Müllerian hormone) is produced by small growing follicles and is a rough marker of ovarian reserve (not perfect, but useful clinically).
13 — Common conditions (short list)
PCOS, endometriosis, uterine fibroids, adenomyosis, PID, ovarian cysts, ectopic pregnancy, premature ovarian insufficiency, menopause, and gynecologic cancers (ovarian, cervical, endometrial). Screening (Pap smears, HPV testing) and prevention (HPV vaccine) matter.
14 — Lifestyle & practical tips
Track your cycle if you want predictability or to chart fertility. Apps help but aren’t perfect.
Maintain healthy weight, avoid smoking, moderate alcohol, manage stress.
If trying to conceive: avoid hot tubs for partners, optimize diet, check meds, consider preconception folic acid (400 mcg daily) to reduce neural-tube defects if pregnancy is possible.
For menstrual pain or heavy bleeding: nonsteroidal anti-inflammatories (e.g., ibuprofen) can help; see a doc for persistent severe symptoms.
15 — Advanced science extras (short)
Oocyte quality & age: eggs accumulate more chromosomal errors with age; aneuploidy risk rises with maternal age.
Assisted reproductive tech: IVF harvests eggs, fertilizes in lab, returns embryos; ICSI helps with severe male factor. Preimplantation genetic testing (PGT) can check embryos for chromosomal problems.
Endometrial receptivity and embryo–maternal signaling are active research areas — implantation is more than stickiness, it’s a molecular handshake.
Immunology: the maternal immune system adapts to tolerate the fetus; autoimmune disease can complicate this balance.
Menopause & HRT: menopause = permanent end of menses after 12 months without period; hormone replacement therapy (HRT) can manage symptoms in appropriate patients.
Final summary (TL;DR again)
The female reproductive system is a coordinated set of ovaries, tubes, uterus, cervix, vagina, and external genitalia plus the nervous and endocrine networks that control cycles, sexual response, and pregnancy. Eggs are finite and age matters. Ovulation, fertilization (usually in the fallopian tube), and implantation in the uterus are the central steps for conception. Hormones — especially estrogen and progesterone — run the show, and many medical and lifestyle factors can help or hurt fertility and sexual function.